Final examination General medicine short case
This is an online E-log book to discuss our patients de-identified health data shared after taking his /her/ guardian informed consent here we discuss our individual patients problems through series of input from available global online community of experts with an aim to solve those patients clinical problems with collective current best evidence based inputs.
Date of admission - February 3
43 year old female patient presented to the opd with chief complaints of low backache since 2 days, vomitings and pain in the abdomen since 1 day.
History of present illness-
Patient was apparently asymptomatic since 6 years back , then she had anasarca for which she was admitted in hyderabad. There she was diagnosed with hypothyroidism (tab. Thyronorm 50 micrograms ),renal failure (tab. Torsemide 20 mg+spironolactone50mg) and diabetes mellitus for which she was on injection Mixtard and increased in doses since 1 and half year.
Now she presented to the opd with pain in the abdomen which is of diffuse ,intermittent ,dull aching pain associated with vomitings 2 episodes a day which is of non billious, non projectile and contains food particles.
No history of fever, cold, cough ,constipation, loose stools.
No history of pedal oedema, reduced urineoutput, facial puffiness.
Past history-
Patient has diabetes mellitus since 6 yrs and on medication-injection MIXTARD 20 units intially which is increased to 25 units one and half year back.
Hypothyroidism since 6 yrs and on medication tab. Thyronorm 50 micrograms.
Personal history :
Diet - mixed
Appetite - decreased
Sleep - adequate
Bowel movements : regular .
Bladder movements : regular.
No addictions.
Family history:
Her mother is a known case of diabetes mellitus.
Menstrual history:
Menopause since 2 yrs.
General examination-
Patient is conscious, coherent and cooperative well oriented to time, person and place.
Physical examination-
No pallor
No icterus
No cyanosis
No clubbing of fingers
No generalised lymphadenopathy
Moderate dehydration is present.
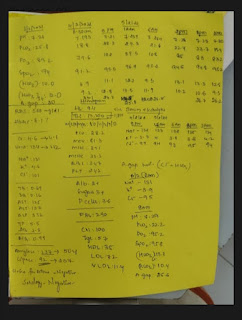
Vitals-







Comments
Post a Comment